Rose (not real name), a 15-year -old girl of school going age, is now eight
months pregnant and about to deliver after being allegedly defiled by a
paternal uncle. Being an orphan with no immediate family to turn to, she
struggles daily to find decent shelter and meet her basic needs. While she
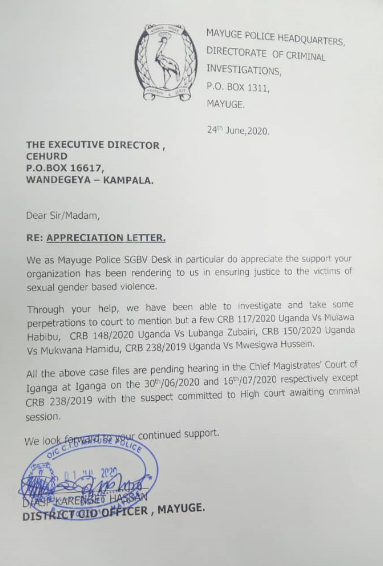
stays in the care of a well-wisher, her case was only reported to the Police
when she was five months pregnant. The delay in reporting her case was
caused by the alleged offender who has threatened the life of Rose and
anyone that attempts to provide shelter and seek justice for her.
Rose is a classic example of many girls whose stories have been
normalised in our societies. They barely see the light in the corridors of
courts of justice due to other contributing factors that have resulted into
immense physical and mental traumatic suffering.
Many children and young people are yet to receive justice for the abuses
inflicted upon them due to the failure of the different stakeholders playing
their respective roles in the chain of justice.
A gap in access to information
In 2019, 13,613 defilement cases were reported according to the Police
Annual Crime Report. Center for Health, Human Rights and Development
(CEHURD) has so far recorded 21 cases through their Community Health
Advocates and their toll-free line (0800313131). Many of these have not
received sufficient redress from the Police and the Courts of Law. The few
that have been settled out of court, are usually done so in ways that do not
favour the justice needs of the children affected. As such, access to justice
for children in Uganda remains a dream.
Access to sexual and reproductive health and rights (SRHR) information
continues to be among the most controversial and contentious topics in
Uganda’s legal and policy environment. This is because of the competing
approaches in policy debates and legal approaches that range from religious and cultural perspectives that inform our different backgrounds. A combination of factors such as limited access to a wide range of sexuality
information and education for both in and out of school young people, rape,
defilement and poverty continue to account for the numerous teenage pregnancies and child marriages in Uganda.
The lack of information among adolescent girls and young women such as
Rose shows that many of them are not empowered about their SRHR. It
further demonstrates the violence adolescent girls and young women go
through as a result of sexual violence coupled with the lack of SGBV shelters
from where they can receive psychosocial support.
Three out of 10 teenage girls become pregnant before they reach 20 years
of age and over 300,000 babies born in Uganda are born by adolescents
aged 15-19 years. Teenagers in rural areas are more likely to start child
bearing earlier than those in urban areas; 27 per cent and 19 per respectively. It is important to note that one of the major drivers of teenage
pregnancy is an early sex debut among young people. According to the
Uganda Demographic and Health Survey of 2016, 10 per cent of women
and 17 per cent of men have already had their first sexual encounter by the
age of 15.
Pursuing a child-friendly justice system
The current retrogressive regulations and policies coupled with lack of
sexuality education and other reproductive health and rights information and services have exacerbated the already bad state of young people’s health and well being.
As the world commemorates the Day of the African Child today in memory
of the thousands of black school children who took to the streets on June
16, 1976. They did this to protest the inferior quality of education and to
demand their right to be taught in their language. This is therefore a good
opportunity to not only create awareness about the needs of young people
but also to assess the state of their rights in Africa. It is also a good time to
amplify the need for a continued improvement in their education. The day
draws attention to the lives of African children and encourages people’s spirit of abundance to share something special with a child in Africa.
The Constitution of the Republic of Uganda defines a child as any one
below the age of 18 years. This year’s theme, “Access to a child- friendly
Justice system in Africa”, reminds us of the restrictions that our current
policies have. It is also an opportunity for duty bearers to help the Ugandan
child enjoy their right to access to friendly justice, sexuality education and
other health information and services. This access would counter the
problems of unplanned pregnancies, pregnancy related complications and
unsafe abortions that account for a sizable contribution to the maternal
mortalities in adolescent girls and young women. The outbreak of the
COVID-19 global pandemic and its rapid spread throughout the world,
Uganda inclusive, came with increased risk for the population, especially
young people.
The pandemic has equally put many health care systems to the test on the
competence of responding and containing the virus while observing human
rights, particularly the rights of young people.
In Uganda, the state’s response to minimise the spread, has been slow to
address sexual and reproductive health, maternal health, access to justice
and other needs of young people. This is further reflected by the supplementary budget allocations being requested by the institutions of
government to respond to the pandemic. Many of these barely have any
consideration for health and human rights.
Just a few weeks into the outbreak, access to services was already
problematic as a number of rights violations were cited. Numerous media
reports about teenage pregnancies, violence against children, defilement,
and rape, among others were and continue to be reported. All this has been
exacerbated by the lock down as imposed by the President of Uganda which
also caused temporary halting of court proceedings. This has further slowed down the speed at which young people can access justice during this time.
Meanwhile, they continue to experience human rights violations.
This comes at a time when the country continues to grapple with poor SRHR
indicators. This means that young people in and out of school continue to
bear the burden of these negative SRHR indicators. This burden includes
teenage pregnancies, problems accessing essential health commodities like
menstrual health products such as sanitary pads, HIV/AIDS and other STIs
medication, among others. Some of the factors that have contributed to this
state of affairs include the lack of information for young people to enable
them make informed health choices, lack of access to services and all these
are exacerbated by the weak policy and legal environment.
Recommendations
To undo this harm and correct the above indicators, the government needs
to take bold steps in establishing progressive laws and policies that are
aimed at eliminating the various injustices that continue to affect Uganda’s
children;
- Fast track the passing of the National Policy on Sexual and
Reproductive Health and implement the recently approved Age Appropriate Sexuality Education National Framework. - Fast track the effective implementation of the National strategy on
ending child marriage and teenage pregnancies in Uganda of 2015 - Develop comprehensive multi-sectoral strategies to avert the
challenges and injustices that continue to ruin lives of children and young people and harmonise legislation on marriage to provide for 18 years as the minimum legal age for marriage. - Strengthen the enforcement of laws against defilement, rape and
other forms of child abuse and establish youth friendly spaces at health units. - Facilitate the Courts of Law to hear and determine cases defilement,
rape and other forms of child abuse to enable children access justice timely. - Finalise and pass the Adolescent Health Policy to update issues of
adolescent health in national and global development trends and context. - Government establishes provisional shelters at police stations manned by the Child and Family Protection Unit, to avail SGBV survivors temporary accommodation pending medical examination and investigation of cases to avoid frustrations.
- That the government ensures that children have access to psycho social support to meet their mental health needs. Train senior women and male teachers on how to provide counselling and deal with the different health needs of young people, including implementation of the Girl Child School Re-entry and Retention Strategy to give any girls who may report to school with pregnancies, an opportunity to continue with their studies.
- Repeal all those laws and policies that compromise the protection and
welfare of the children.
In a nutshell, as we celebrate the Day of the African Child, creating a child-
friendly justice system in Africa, and specifically in Uganda, requires a multi sectoral approach and meaningful collaborations. This collaboration should not only be among the different government line ministries and agencies but also with civil society organisations, parents, teachers and the media.
A version of this article was originally published in the Daily Monitor.